A mild fever after a tooth extraction is fairly common and usually nothing to worry about. It often happens within the first day or two as your body’s immune system responds to the procedure and begins the healing process.
If a fever continues, climbs above 100°F (38°C), or is paired with other troubling symptoms, it could point to an infection or another complication.
It helps to know when a mild fever is normal and when it signals something more serious. Paying attention to your body and following the dentist’s aftercare advice makes recovery smoother and lowers the risk of problems. In the sections ahead, we’ll look at why fever can happen after a tooth is removed and what signs should not be ignored during healing.
At Sunrise Mall Dental, we are here to guide you through everything you need to know about fever after a tooth extraction—what’s normal, what’s not, how to manage it, and when to call your dentist.
Why Fever Occurs After Tooth Extraction
A tooth extraction is essentially minor surgery. Anytime the body goes through a surgical procedure, the immune system jumps into action. Part of that immune response can involve a slight rise in body temperature.
Fever after a tooth extraction can occur for several reasons. It’s often the body’s natural response to healing, but it can also be a sign of something more serious, such as an infection. Knowing why a fever can happen after a tooth extraction helps you manage healing and spot when to seek medical care.
Normal Inflammatory Response
After a tooth extraction, the body triggers inflammation to begin healing the wound. This process can cause a mild fever, usually under 38°C (100.4°F). The immune system increases blood flow to the area, bringing cells that fight germs and repair tissue.
This reaction may also cause tiredness or body aches. The fever is generally short-lived and should lessen after two to three days. Using prescribed pain relievers and cold packs can ease discomfort. Mild swelling and some warmth at the extraction site are normal parts of this response.
Infection Risks and Dry Socket
A fever that stays high or worsens could mean an infection around the extraction site. Bacteria can enter the open wound, causing redness, pus, severe pain, and swelling that does not improve.
Dry socket is a common complication where the blood clot getting dislodged exposes bone and nerves. This condition often causes intense pain and sometimes fever. Signs of infection or dry socket include persistent fever, bad smell, and increased discomfort after the first few days.
If infection or dry socket is suspected, professional dental care is needed for treatment such as antibiotics or cleaning.
Systemic Reactions to Surgery
The physical and emotional stress from tooth extraction can affect the whole body. Stress responses may weaken the immune system temporarily, making fever or flu-like symptoms more likely.
Some medications used after surgery, like antibiotics or painkillers, may cause side effects such as nausea or fatigue that mimic fever symptoms. Additionally, dehydration from eating less or drinking less due to soreness can make feverish feelings worse.
Managing stress, staying hydrated, and following medication guidelines help reduce these systemic effects during recovery.
For more detailed information about why fever happens after a tooth extraction, visit Flu-Like Symptoms After Tooth Extraction at Knox County Hospital.
When Fever Is Normal and When It’s Not
Not all fevers mean something serious. Here’s how to tell the difference between a harmless, short-term fever and one that needs medical attention:
Normal Fever
A slight fever (under 100.4°F) right after the extraction is usually just your body healing itself. It’ll probably show up in the first day or two and should fade pretty quickly.
- Temperature below 100.4°F (38°C)
- Lasts only 24–48 hours after surgery
- No other severe symptoms
- Goes away with rest and fluids
Concerning Fever
If the fever reaches or exceeds 100.4°F and lasts more than 48 hours, it may signal an infection. Fever at this level often comes with other signs, like swelling or pain that gets worse instead of better.
Monitoring temperature regularly after surgery can help detect abnormal changes early. Any high or prolonged fever should be taken seriously and evaluated by a dentist.
- Temperature above 101°F (38.3°C)
- Persists for more than 2 days
- Comes with worsening pain, swelling, or discharge
- Spreads beyond the mouth (chills, body aches, difficulty swallowing or breathing)
Additional Signs of Complications
Beyond fever, several symptoms suggest complications like infection or dry socket. Watch for:
- Severe, throbbing pain starting 2–3 days post-extraction
- Increasing swelling beyond 48 hours
- Pus or foul-smelling discharge from the extraction site
- Redness and tenderness in the gums
- Bad taste or bad breath that doesn’t improve
- Swollen lymph nodes near the jaw or neck
Dry socket, which results from the loss of the protective blood clot, causes intense pain but usually no fever unless infection follows. Recognizing these signs helps differentiate normal healing from problems.
When to Seek Medical Attention
Immediate dental care is necessary if symptoms worsen or any of the following occur:
- Fever over 100.4°F lasting more than two days
- Persistent or increasing pain after 48 hours
- Swelling spreading to the face or neck
- Pus or persistent bleeding beyond 24 hours
- Difficulty swallowing, breathing, or opening the mouth
Prompt treatment can prevent serious infections or complications like osteomyelitis. When uncertain about symptoms, contacting a dental professional ensures proper evaluation and care.
Preventing and Managing Fever After Tooth Extraction
It is most important proper care and attention after a tooth extraction lower the risk of infection, fever, and other problems. Keep the site clean, avoid risky habits, and watch for swelling or pain. If issues like dry socket show up, early treatment can speed recovery.
Post-Extraction Care Practices
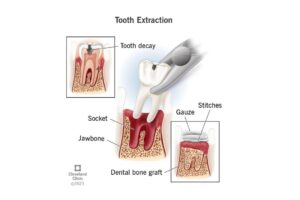
After tooth extraction, maintaining the blood clot at the extraction site is crucial. This clot protects the wound and helps healing. Patients should avoid rinsing their mouth forcefully or spitting for the first 24 hours. Eating soft foods and not using straws can prevent dislodging the clot.
Oral hygiene should be gentle but consistent. Brushing away from the extraction site and rinsing with saltwater after 24 hours kill bacteria without disturbing healing tissue. Pain and swelling can be managed with prescribed medication and ice packs.
Following the dentist’s aftercare instructions reduces irritation that might cause a low-grade fever. Rest and hydration support the body’s healing process naturally.
Reducing Infection Risks
Infections are a common cause of fever after tooth extraction. Bacteria entering the wound can lead to swelling, pus, or fever above normal levels. To reduce infection chances, patients should avoid smoking or drinking through straws for at least a week.
Using antibiotics as prescribed by the dentist helps prevent or control infection, especially in patients with weaker immune systems. Avoid touching the extraction site with fingers or tongue, which can introduce germs.
Monitoring for symptoms such as increasing pain, redness, or persistent fever is important. If these signs appear, prompt dental consultation is necessary to treat any infection before it worsens. Cleaning the mouth gently and keeping follow-up appointments ensure healing stays on track.
Managing Dry Socket Effectively
Dry socket is a painful condition after tooth extraction caused by the loss of the blood clot. It exposes bone and nerves and often leads to severe pain, bad breath, and possible fever if infection follows.
Preventing dry socket involves not disturbing the clot by avoiding smoking, spitting hard, or vigorous rinsing. Eating soft foods and resting can help the clot stay in place.
If dry socket develops, dental treatment is needed. Dentists apply medicated dressings to reduce pain and protect the area. They may also provide pain relief and instructions to keep the socket clean. Treating a dry socket early can prevent fever and speed healing. For details on infection control and recovery, see this post-extraction infection and care guidance.
Tips to Prevent Fever After a Tooth Extraction
The best way to deal with post-extraction fever is to avoid it altogether. Prevention starts with good aftercare:
- Take prescribed antibiotics (if given). Finish the full course even if you feel better.
- Don’t touch the wound. Avoid poking it with your tongue, finger, or anything else.
- Keep your mouth clean. Rinse gently with warm salt water after the first day. Avoid mouthwashes with alcohol.
- Follow a soft food diet. Stick with soups, smoothies, scrambled eggs, and avoid hard or crunchy foods that can disturb the clot.
- Don’t smoke or vape. Nicotine reduces blood flow to the gums and delays healing.
- Avoid alcohol. It interferes with healing and may react with pain medications.
Recovery Timeline and Monitoring Progress
Tooth extraction recovery happens step by step, with predictable signs along the way. Watching for changes in symptoms helps identify whether recovery is on track or if a fever or other issues indicate complications.
Expected Healing Milestones
In the first 24 hours, a blood clot forms in the extraction socket to protect the bone and nerves. Bleeding usually slows and stops during this period. Swelling and mild pain peak within 48 to 72 hours and then start to decline.
By day 3 to 5, swelling should reduce significantly, and discomfort lessens. The gum tissue begins to close over the socket. Most people can eat soft foods and start gentle mouth rinses after 24 hours, with dentist approval.
Around one week after extraction, the wound starts to fill with new tissue. Pain typically fades entirely. Normal activities and diet can often resume, but some deeper healing inside the bone continues for several weeks.
Tracking Symptoms and Improvements
It is important to track symptoms like pain, swelling, and especially fever after tooth extraction. A low-grade fever (up to 100.4°F or 38°C) in the first day or two is common and usually not concerning.
If fever persists beyond 48 hours or rises above 101°F (38.3°C), this may signal infection. Other warning signs include worsening pain, increased swelling after day 3, foul taste or smell, and continuous bleeding.
Patients should watch their healing each day and reach out to their dentist if symptoms get worse or new ones appear. This helps manage conditions like dry socket or infection early.
FAQs :
1. Is it normal to have a fever after tooth extraction?
Yes, a low-grade fever (below 100.4°F) within the first 24 hours is fairly common and usually not a cause for concern.
2. How long does a fever last after tooth extraction?
Most mild fevers go away within 1–2 days. If your fever lasts longer than 48 hours, consult your dentist.
3. Does wisdom tooth removal cause more fever than other extractions?
Wisdom tooth extractions are often more complex and may lead to more swelling and inflammation, making fever slightly more common.
4. Can antibiotics prevent fever after extraction?
Antibiotics can help reduce the risk of infection, but they don’t guarantee prevention. Only take them if prescribed by your dentist.
5. Should I go to the ER for a fever after a tooth extraction?
Go to the ER if your fever is very high, comes with severe swelling, difficulty breathing, or spreading infection symptoms.
6. What foods help recovery after a tooth extraction?
Soft foods like yogurt, smoothies, oatmeal, mashed potatoes, eggs, and soup are gentle on the healing area and support recovery.
7. Could a fever after dental surgery indicate an infection?
Yes, a high or prolonged fever can be a sign of infection. Other symptoms often accompany it, such as swelling or increased pain.




